Regular veterinary check-ups are paramount for monitoring renal function. Blood tests and urinalysis provide insights into organ performance, guiding dietary and medical interventions.
Incorporating a specialized diet designed for renal support can significantly enhance well-being. These formulas often contain controlled protein levels and added omega-3 fatty acids, essential for reducing inflammation and promoting kidney health.
Hydration plays a critical role in maintaining optimal kidney function. Encouraging water intake through wet food or water fountains can help prevent further complications. Always keep freshwater accessible and consider flavoring it with a bit of low-sodium broth to entice reluctant drinkers.
Medication may be necessary to manage symptoms and slow progression. Phosphate binders and antihypertensives are commonly prescribed to address specific issues related to renal insufficiency.
Regular monitoring of weight and appetite is vital. Adjustments to feeding routines may be needed based on the cat’s response to the dietary changes. Keeping a log of food intake and behaviors can assist veterinarians in tailoring the treatment plan.
Exploring supportive therapies, such as subcutaneous fluids, can provide additional hydration and alleviate stress on the kidneys. This approach can be beneficial for cats that struggle with oral hydration.
Finally, maintaining a stress-free environment contributes positively to overall health. Gentle play, companionship, and a quiet space can enhance quality of life for those facing renal challenges.
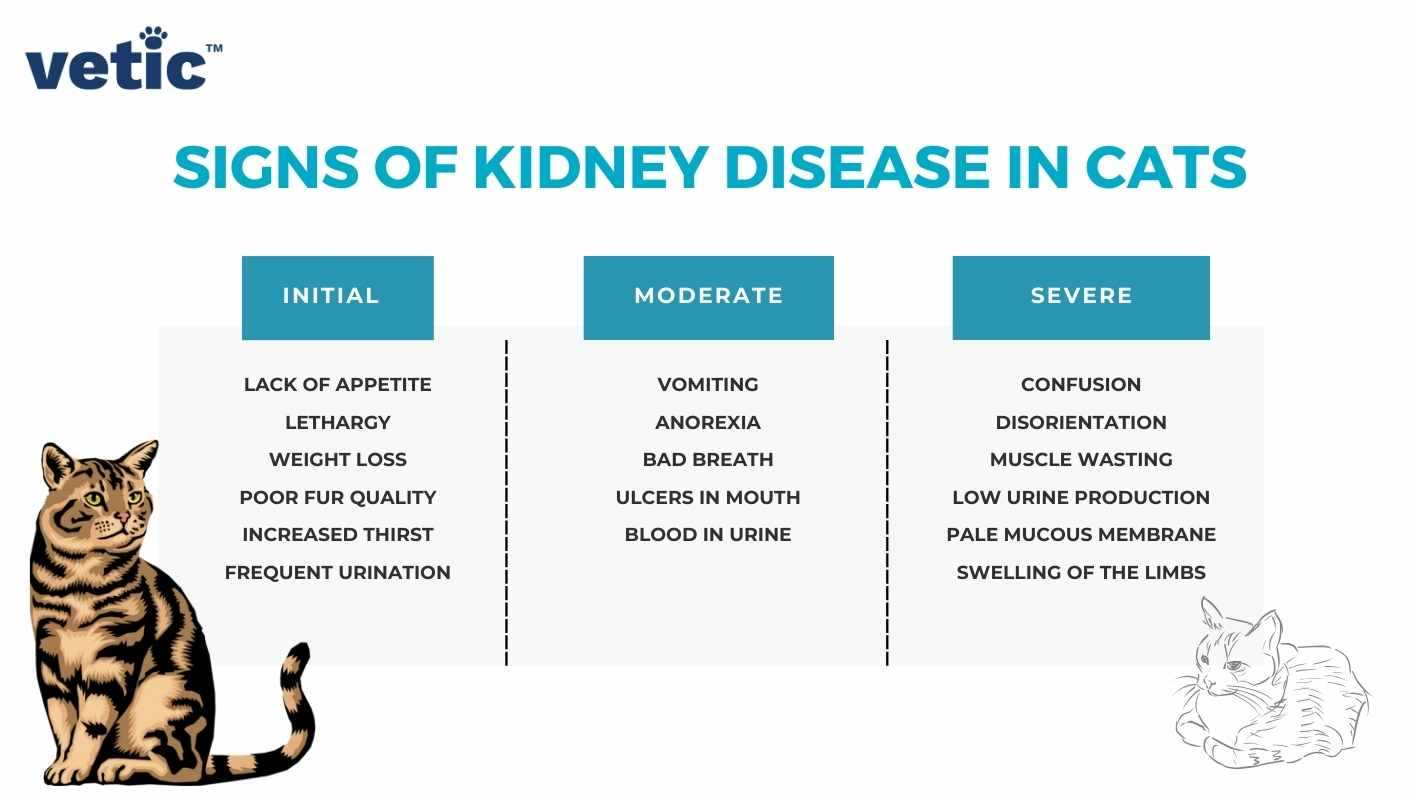
Understanding the Stages of Kidney Disease in Cats
Recognition of the different phases of renal impairment is key. There are typically four stages, each characterized by the severity of the condition and the associated symptoms.
Stage 1 is often subtle, with minimal clinical signs. Routine check-ups may reveal reduced kidney function through blood tests. Monitoring is crucial here, as lifestyle changes can help manage progression.
Stage 2 presents more noticeable symptoms such as increased thirst and urination. At this point, dietary adjustments and regular vet visits become essential to help maintain quality of life.
In Stage 3, symptoms worsen. Weight loss, vomiting, and lethargy may occur. This stage often requires more intensive management strategies, including fluid therapy and medications to support kidney function.
Stage 4 is critical, with severe symptoms impacting daily life. Palliative care becomes a focus, aimed at comfort rather than cure. This stage often leads to difficult decisions regarding treatment options.
Throughout all stages, keeping up with preventive care is important. For example, using the best oral flea treatment for cats without vet prescription can help avoid additional health complications.
Monitoring changes in behavior and health is vital at all stages. Early intervention can make a significant difference in managing the condition effectively.
Dietary Modifications for Cats with Kidney Issues
Limit protein intake to high-quality sources. Opt for easily digestible options such as chicken, turkey, or fish. This approach reduces the burden on failing organs while still providing necessary nutrients.
Incorporate low phosphorus content foods. Excess phosphorus can worsen renal function. Look for specialized diets designed specifically for compromised function that have controlled phosphorus levels.
Increase water consumption. Hydration is key. Wet food or adding water to dry kibble can encourage fluid intake, supporting overall health. Consider a cat water fountain to entice drinking.
Adjust sodium levels. A low-sodium diet can help manage blood pressure and reduce the risk of fluid retention. Check the labels for sodium content in commercial foods.
Supplementation
Consider omega-3 fatty acids, which may have a protective effect on the kidneys. Fish oil supplements or specialized diets can provide these beneficial fats.
Consult a veterinarian about antioxidant supplements, such as vitamins E and C. These can help combat oxidative stress and may support renal health.
Regular Monitoring
Routine check-ups are crucial. Regular blood tests assess kidney function and tailor dietary modifications accordingly. Keeping track of changes in appetite, weight, or behavior can guide adjustments in nutrition.
Medications and Supplements for Kidney Disease Management
Renal support medications play a significant role in managing conditions affecting the urinary system. Phosphate binders, such as aluminum hydroxide or lanthanum carbonate, help control phosphorus levels, preventing further complications. These should be administered with meals to enhance absorption and effectiveness.
Fluid Therapy

Subcutaneous fluids provide hydration and assist in flushing out toxins. Administering these fluids can be done at home, offering convenience for both the feline and the caregiver. Regular monitoring of hydration status remains crucial to assess the effectiveness of this treatment.
Supplements
Omega-3 fatty acids, derived from fish oil, contribute to reducing inflammation and promoting kidney health. Antioxidants, such as vitamin E and coenzyme Q10, also support overall well-being and may slow the progression of the condition. Always consult with a veterinarian regarding appropriate dosages and potential interactions with other medications.
Hydration Strategies for Feline Renal Concerns
Encouraging water intake stands out as a primary method for managing renal issues. Providing fresh water daily, preferably in multiple bowls throughout the home, promotes hydration. Cats often prefer running water, so a pet water fountain can be a great addition, enticing them to drink more.
Incorporating wet food into their diet significantly enhances fluid intake. Look for high-quality canned options with a high moisture content, ensuring they receive both nutrition and hydration. Mixing water or low-sodium broth into dry kibble can also help increase fluid consumption.
Flavor Enhancements
Enhancing water with flavor can make it more appealing. Adding a splash of tuna juice or chicken broth can encourage drinking. Always ensure any added ingredients are free from harmful additives like onion or garlic.
Monitoring Hydration Levels
Regularly check for signs of dehydration, such as dry gums or skin elasticity. A simple pinch test can help; if the skin doesn’t spring back quickly, it might indicate dehydration. Keeping track of water intake can provide insights into hydration status, helping to adjust strategies as needed.
Monitoring Progress and Symptoms in Affected Cats
Regular observation of behavior and physical condition provides valuable insights. Keep track of appetite, hydration levels, and litter box habits. Note any changes in weight or energy levels, as these can indicate shifts in well-being.
Key Symptoms to Watch
Excessive thirst or urination, vomiting, and changes in grooming habits demand attention. If there’s a noticeable increase in lethargy or signs of discomfort, prompt evaluation is necessary. Monitoring dental health is also crucial, as oral issues can arise with renal complications.
Utilizing Veterinary Visits
Routine check-ups enable timely adjustments to care plans. Blood tests and urinalysis offer concrete data on kidney function, supporting informed decisions. Discuss any emerging concerns with the veterinarian to tailor management strategies effectively.
For those managing aquatic environments, I found this helpful resource: how to keep fish tank warm in power outage.
When to Consider Advanced Treatments or Palliative Care
Advanced interventions become relevant when a feline’s condition deteriorates despite standard care. Signs indicating this include:
- Persistent vomiting or nausea that doesn’t respond to anti-nausea medications.
- Severe weight loss and muscle wasting, especially if accompanied by lethargy.
- Difficulty breathing or signs of fluid buildup in the abdomen or lungs.
- Frequent urination paired with increased thirst and inability to maintain hydration.
- Refusal to eat for more than 24 hours, indicating a significant decline in health.
At this stage, discussing options such as:
- Subcutaneous or intravenous fluid therapy for hydration and electrolyte balance.
- Advanced imaging like ultrasound or X-rays to assess internal issues.
- Specialized medications targeting symptoms or complications.
Palliative care becomes a priority when comfort is paramount. Key aspects include:
- Ensuring a quiet, comfortable space away from stressors.
- Administering pain relief and anti-nausea medications as prescribed.
- Focusing on favorite foods and treats to maintain nutrition and pleasure.
Regular consultations with a veterinarian are crucial during this phase to adjust care plans based on the feline’s changing needs. Quality of life assessments can guide decisions, ensuring that the focus remains on comfort and dignity.
FAQ:
What are the common treatments for kidney disease in cats?
Treating kidney disease in cats typically involves a combination of dietary management, medications, and supportive care. A special diet that is low in protein and phosphorus can help reduce the workload on the kidneys. Vet-prescribed medications may include phosphate binders to control phosphorus levels, anti-nausea drugs, and supplements like potassium or vitamin B. Additionally, regular veterinary check-ups are essential to monitor the cat’s condition and adjust treatments as necessary. Some cats may also benefit from fluid therapy to prevent dehydration and support kidney function.
How can I support my cat with kidney disease at home?
Supporting a cat with kidney disease at home involves several practical steps. First, ensure your cat has access to fresh water at all times, as hydration is critical for kidney health. Offering wet food can also help increase fluid intake. Creating a stress-free environment is important, as stress can exacerbate health issues. You can also monitor your cat’s appetite and behavior, noting any changes that may indicate a decline in health. Regular communication with your veterinarian is key; they can provide advice tailored to your cat’s specific needs and suggest home care strategies, including potential adjustments to diet or medications.